Marcus Tatum is combining his background in biomedical engineering with new industrial and systems engineering skills to improve surgical outcomes. His work minimizes risk for vulnerable patients by addressing the lack of surgical simulation and developing new imaging technologies.

Tatum received a master’s degree in biomedical engineering and decided to pursue a PhD in industrial and systems engineering (ISE).
“I really enjoyed the [ISE] classes, there were way more options to choose from,” he said. “I had taken as many biology classes as I wanted and I got a lot of new skills out of the industrial engineering courses. There’s a lot of coding and mechatronics.”
Tatum is a PhD student in the industrial and systems engineering department and a graduate research assistant for the University of Iowa Orthopedic Biomechanics Lab (UIOBL). The lab focuses on addressing clinically-oriented research problems across the wide spectrum of musculoskeletal biomechanics. Tatum has worked closely with the UIOBL researcher team on the following projects.
Using simulation to treat pediatric elbow fractures
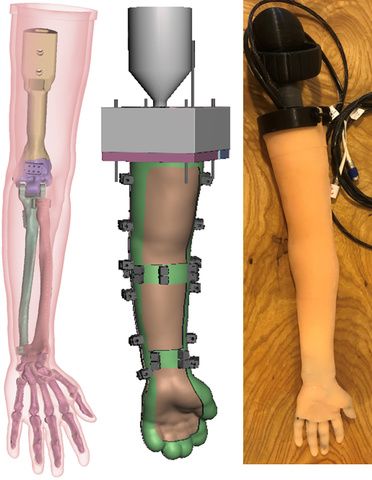
Medical simulators help train surgical residents while minimizing risk to real life patients, allowing residents to learn new skills in a safe environment. Tatum says there are not many simulation opportunities for pediatric operations. In this project, Tatum and fellow researchers developed a simulation for the most common type of fracture that requires surgery in children—supracondylar humerus—or elbow fractures.
The simulator Tatum and co-researchers worked on is focused on the process of fracture reduction, or putting broken bones back together. The simulation device contains 3D-printed broken bones inside of a silicone skin and a surgical drill with a tracking sensor. Using this, residents can practice the entire procedure from start to finish. The tracking system provides X-ray imaging for procedure guidance, tracks the tool as well as bone fragments, and gives an automated assessment of the surgeon’s performance.
Once the procedure is complete, residents get to look at the data: their simulation time, reduction accuracy and efficiency, image use, surgical tool to bone interaction, and surgical wire placement. Tatum says their testing shows promising results, as residents are able to learn fundamental skills in a practice setting.
“With the simulator, we can look at the performance and say to residents, ‘Hey, you need to work on these things before you operate.’ Like with anything, making mistakes is the learning process, so we want these mistakes to be made on the simulator, not the vulnerable patient,” said Tatum.
| 
|
Using surgical X-rays to determine the location of bones in 3D space
This research is focused on patients diagnosed with hip dysplasia. Hip dysplasia is the condition in which the ball portion of the hip joint does not correctly fit into the hip socket. Tatum says that oftentimes patients having surgery for this condition are young, typically in their twenties. Tatum, Geb Thomas, ISE professor, and Don Anderson, professor and lab director at UIOBL, worked to create imaging technology that increases surgical accuracy for this procedure, improving outcomes for these young patients.
Using neural radiance fields (NeRF), Tatum and co-researchers developed near real-time 3D images from 2D fluoroscopy images. Tatum says NeRF was created for rendering new views of photorealistic scenes based on standard camera images. The application of this NeRF algorithm for navigation in orthopedic surgery is unique.
With this technology, there is no need for a preoperative computerized tomography (CT) scan. Surgeons are able to locate bones in 3D space while in the operating room, giving them as much accuracy as possible in ensuring a proper fit in the fracture repair. As imagined, this leads to the best outcomes for young, vulnerable patients.

Tatum’s work is a culmination of his years of both biomedical and industrial and systems engineering. Tatum and the UIOBL researchers are minimizing risk to patients and making strides toward safer surgeries with improved outcomes for young patients.
